Bad data is an expensive problem in many industries, but in the healthcare sector, the stakes are even higher. It’s not just a matter of erroneous records; bad data can directly impact patient care and financial stability. Bad data can significantly slow the process of government reimbursements in healthcare programs such as Medicare and Medicaid, creating a financial bottleneck.
This issue underscores the vital importance of accurate, complete, and standardized healthcare data in speeding up government reimbursement processes. In this article, we will discuss what bad data is and the different ways it can slow down the process of government reimbursements.
What is Bad Data, and How Does it Happen?
Before we can go into how the government reimbursement process can be slowed down by bad data, we have to explain what we mean by bad data. Simply put, bad data is inaccurate, incomplete, outdated, or inconsistent information that can occur where data is collected and used. How does bad data occur? Human error, a system malfunction, outdated software, poor data management procedures, lack of standardization, and even fraud or misrepresentation. In the healthcare sector, bad data can manifest as incorrect patient demographics, erroneous diagnosis or treatment codes, incomplete patient histories, or inconsistent medical records.
Different Types of Bad Data
There are several different types of bad data, and each has its own unique impact on the healthcare reimbursement process:
- Erroneous Data: This type of data refers to information that contains outright mistakes or inaccuracies, such as incorrect patient details or wrong treatment codes, which can misguide healthcare decisions and reimbursement processes.
- Outdated Data: Outdated data is information that was once accurate but hasn’t been updated to reflect recent changes, such as an old address or outdated medical history, leading to potential miscommunication and inaccuracies in health service provision and billing.
- Inconsistent Data: Inconsistent data refers to disparities in the way information is recorded or reported across different sources or systems, creating confusion, reducing interoperability, and potentially leading to flawed decisions or inefficient processes in healthcare.
- Incomplete Data: This is data where some crucial information is missing or only partially recorded, such as a patient’s medical history without recent updates, which can lead to an incomplete understanding of a patient’s health status and potentially affect care provision and reimbursement processes.
- Duplicate Data: Duplicate data refers to redundant or repeated entries of the same information in a database, which can lead to confusion, waste of storage space, and increased difficulty in data management, thus slowing down the reimbursement process.
How Bad Data Slows the Government Reimbursement Process
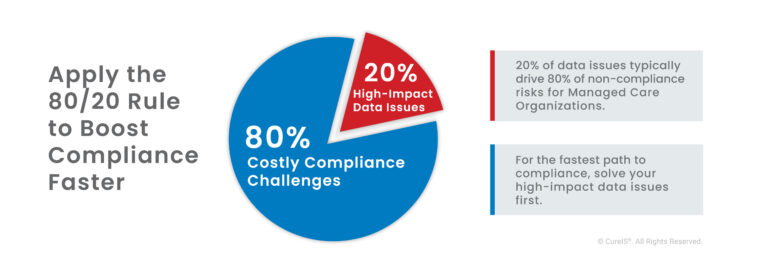
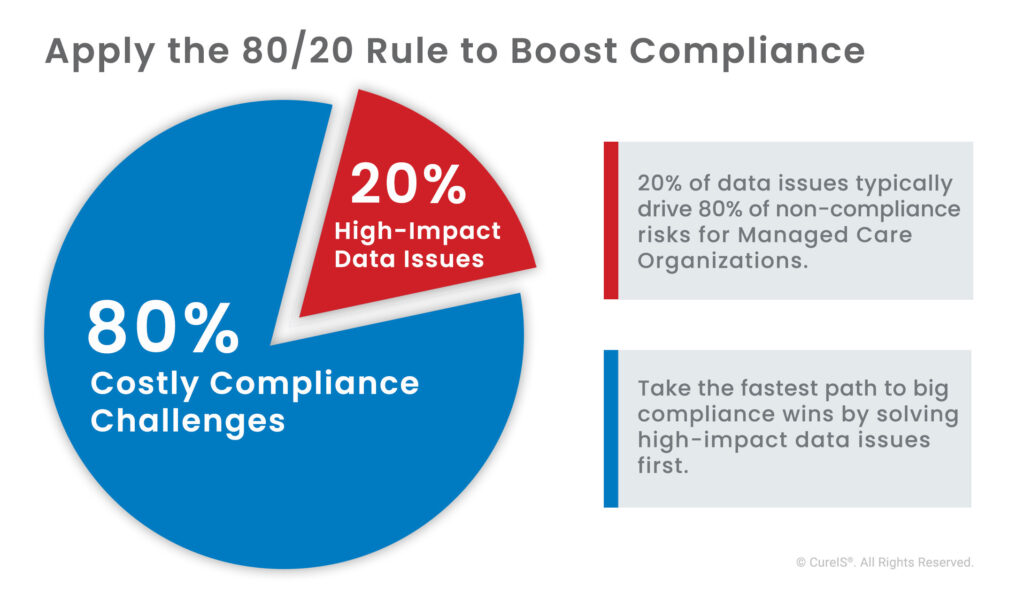
Bad data can create significant obstacles in the government reimbursement process. When reimbursement claims contain errors, are incomplete, or inconsistent, they may be rejected or require additional review, leading to delays or denial of payment. The resources required to identify and correct these errors further slow down the reimbursement process and increase costs.
Bad data can also lead to compliance issues. Government healthcare programs such as Medicaid and Medicare have stringent requirements for accuracy and completeness in reimbursement claims. Non-compliance can result in penalties, loss of eligibility, and even sanctions. Navigating the complexities of these programs with bad data can compound the reimbursement process’s challenges.
Accurate Healthcare Data Speeds Up the Government Reimbursement Process
Accurate and complete data is the backbone of an efficient reimbursement process. With accurate patient demographics, precise diagnosis and treatment codes, and comprehensive patient histories, the chance of claim denial or additional review decreases significantly. This efficiency allows for a faster turnaround time for reimbursement.
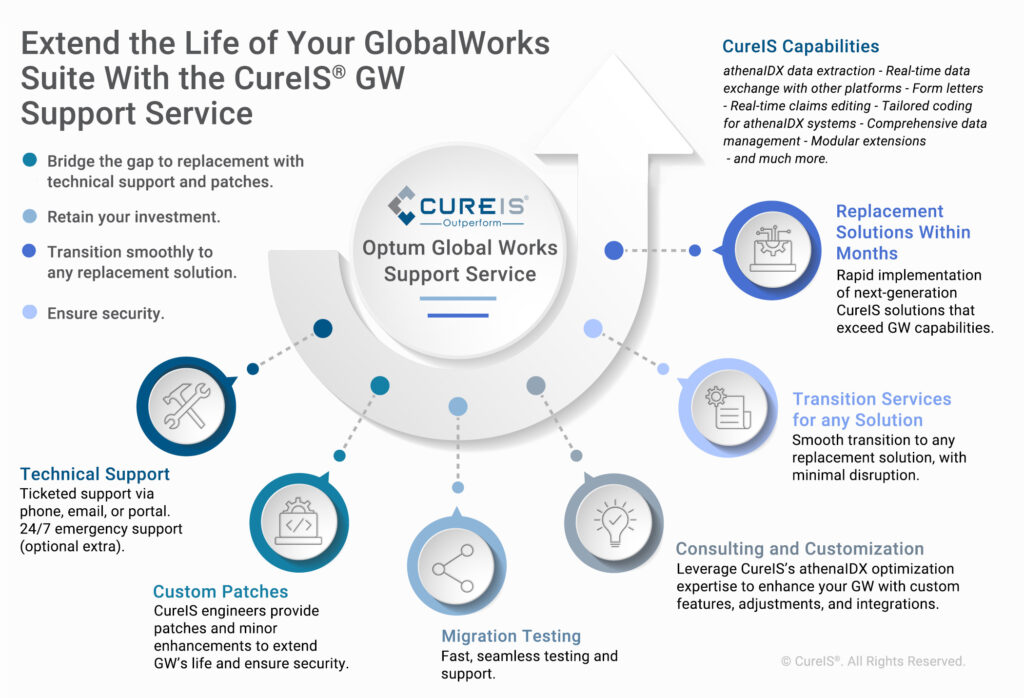
How CureIS Can Help Clean Up Healthcare Data
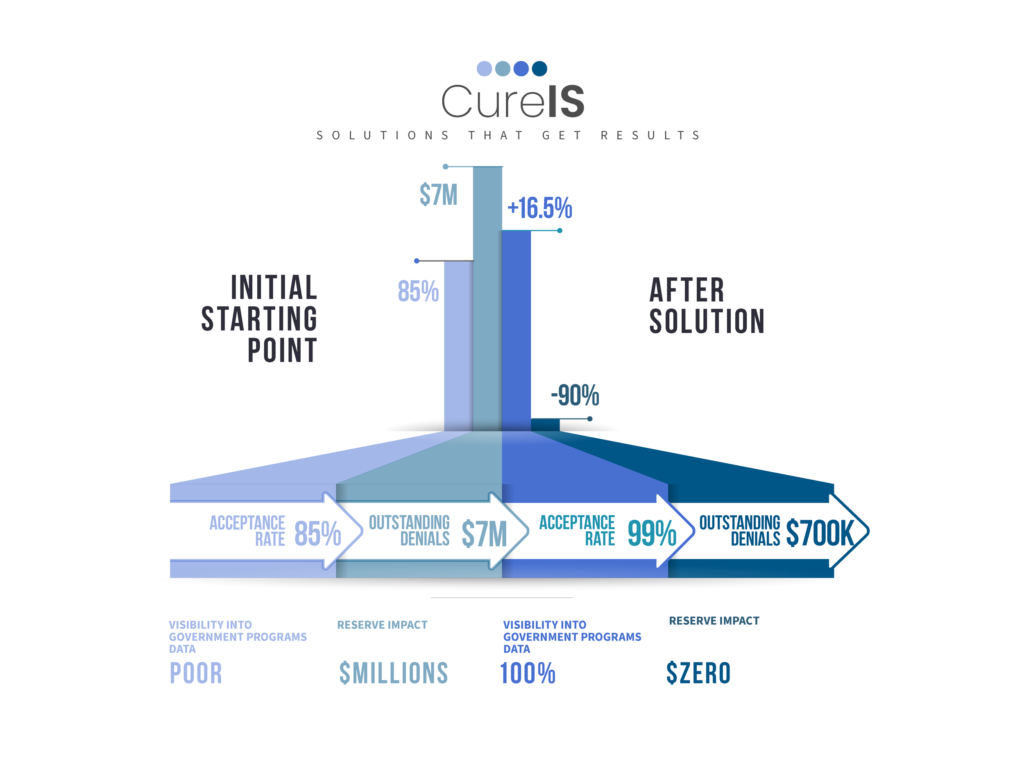
CureIS can make your healthcare operations more efficient by introducing automated processes. We use innovative technology designed to reduce bad data implications, saving you time and money. With our proprietary technology, we apply best practices to your data and automate your business decisions. We take full accountability for business processes that rely on complex data handling and intensive manual workflows.
CureIS turns weeks of data processing into minutes, eliminates the need for large teams, and lowers the risk associated with government program encounters. By cleaning up bad healthcare data, we aim to streamline the reimbursement process.
When CureIS manages your data processes, we take full accountability. We ensure all your data is complete, accurate, and ready to use.
- Faster Turnaround: We can turn weeks of data processing into minutes.
- Less Overhead: You can leverage your team to make critical decisions instead of creating reports and pushing files.
- Lower Risk: We take accountability for implementing your business decisions accurately so that you can focus on your outcomes.
Ready to put an end to the setbacks and mistakes that come from bad data in your reimbursement process? Connect with the experts at CureIS today and find out how our data management solutions can streamline your operations, clean up your data, and speed up government reimbursements. Our team of healthcare data experts is ready to provide the efficiency you need to navigate the complexities of government healthcare programs.