ClaimsCure
Lightning-fast claims adjudication rates
with automated solutions from CureIS.
ClaimsCURE provides a better way to prepare claims for processing.
Navigating claims adjudication is a complex challenge in a landscape of specific and fluid requirements. Members, providers, government programs, commercial carriers, claims processors, and finance teams who are grappling with rejected and misdirected claims can experience significant impacts increasing delays in adjudication, and ultimately cost to the organization.
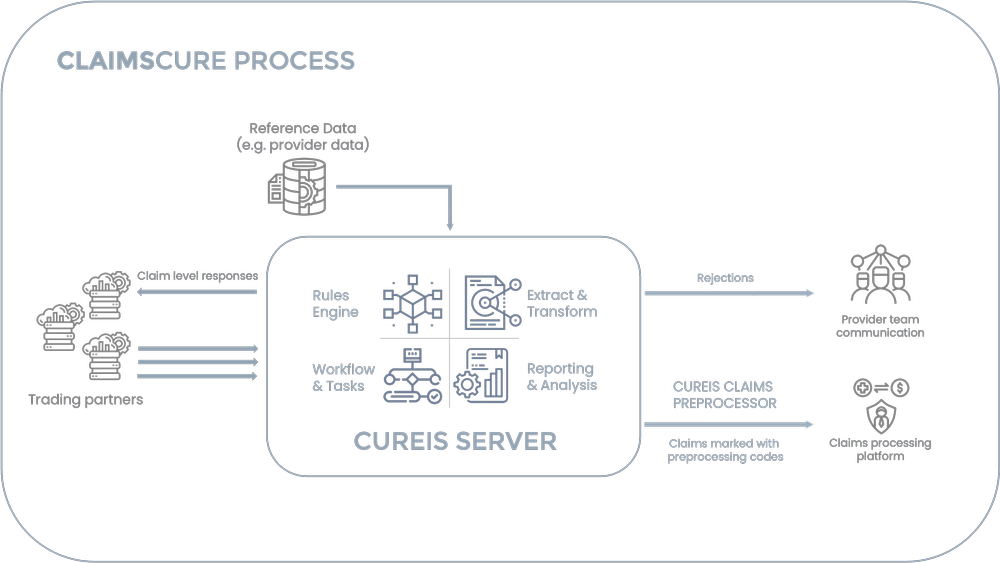
CureIS can help. We consume every inbound claim, check for duplicates, validate the data, ensure the claim is yours, the member is eligible, the providers are approved, the coordination of benefits information is valid, it supports encounter requirements, and all other requirements are met for your adjudication platform to handle it. We automate the management of misdirected claims and can provide clues to your claims system so it can automatically process the claims without manual intervention for most verification processes. We can even automate the transactions for prospective payment processing, eliminating manual processes.
Our CureIS Server ingests reference data from multiple sources to evaluate and manage issues before the claim is processed by your system, ensuring it is ready for efficient processing. Our customers experience dramatic increases in their auto-adjudication rate, along with high encounter acceptance rates, lower provider disputes, and even lower appeal overturn rates. Our workflow, rules engine, and automation free up your team to focus on improvement opportunities, making better decisions for CureIS to automate.
Intelligent automation of pre-adjudication validation processes is crucial for cost management. CureIS supports streamlined process solutions for complex scenarios
while ensuring that the adjudication system is fed accurate and complete data when determining provider payments. ClaimsCURE is a tailored solution that significantly enhances outcomes while reducing costs and improving overall efficiency.
CureIS is fully accountable for ensuring results.
Explore more solutions:
Streamline enrollment processes and determine
eligibility accurately, consistently, and quickly.
Identify any and all missing encounters with enhanced
tracking, management and reporting for Medicare,
Medicaid, and other relevant parties.
Reduce manual data management, accelerate
workflows, and gain operational perspective for
everything from preprocessing data to integrating new
systems to accessing archived data, and more.