EnrollmentCure
Next Level Enrollment
Automates and simplifies even the most complex operations.
Automates and Simplifies Complex Enrollment Options
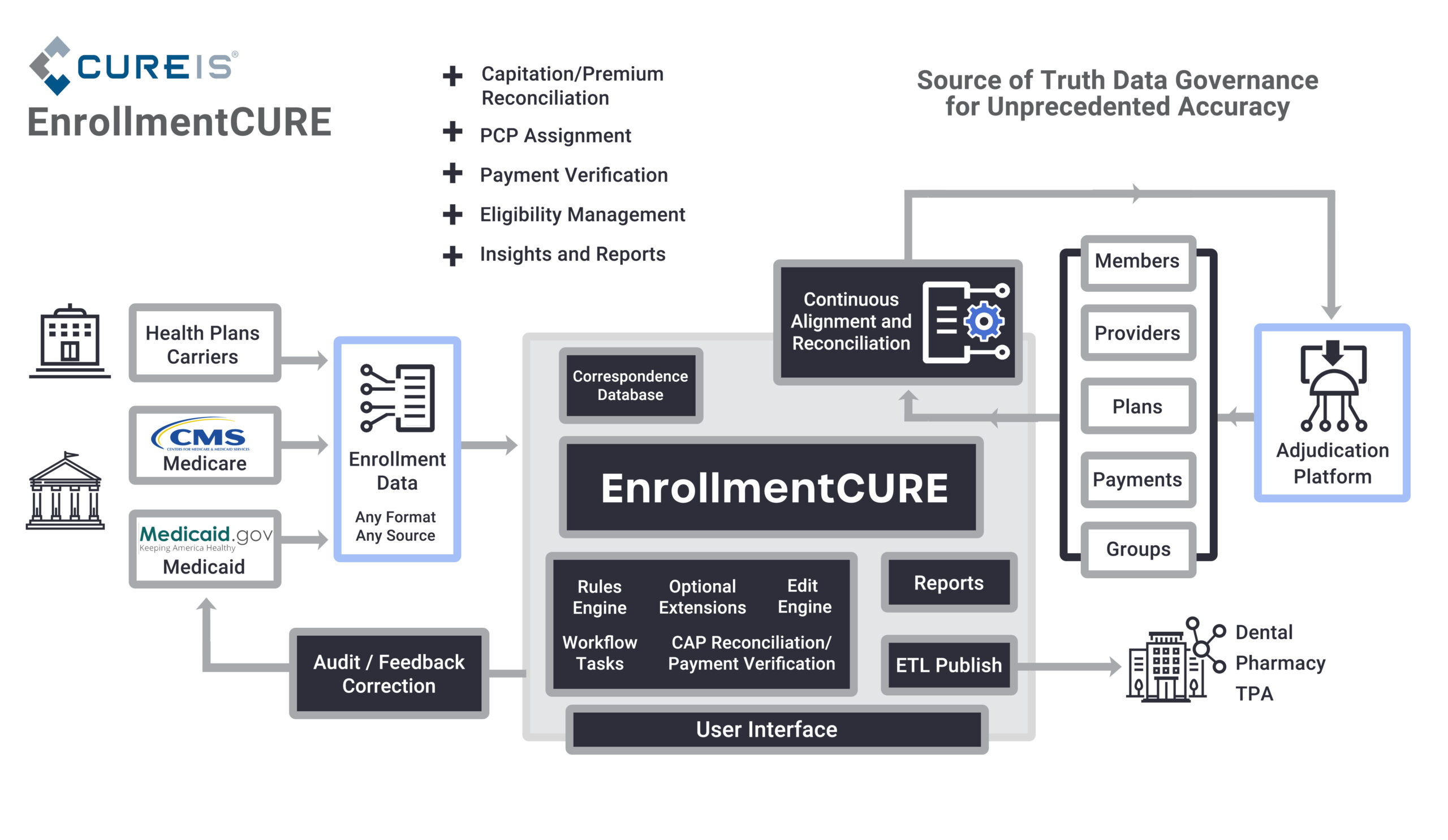
Navigating enrollment challenges should not be a costly grind. CureIS developed EnrollmentCURE to ensure that the critical details of member demographics, benefit plan, and PCP assignment and financial information (such as Premium, Capitation, and Subsidies) are rapidly aligned between the Government/Carrier/Health Plan and the Claims Administration and Processing Systems (CAPS) to ensure members claims are adjudicated accurately and without delay.
Real-time Data for Real-time Decisions
EnrollmentCURE streamlines daily operations by promoting daily activity files that provide timely member data. This translates to accurate copays at the time of the visit, reducing the need to check eligibility outside of core systems.
Swift Implementation
The CureIS team brings years of expertise to enrollment processes. Proven workflows and an extensive menu of business rules and edits enable fast implementation. Changes can be implemented and tested within hours, instead of weeks or months.
Cost-Effective Efficiency
EnrollmentCURE offers a robust set of features, including integration with unlimited data sources, system-agnostic adjudication, and automated processing. Controllable environmental challenges are addressed, lowering operating costs by eliminating downstream issues that result in reprocessing, appeals, or encounter denials.
No Surprises. Just Results
Explore more solutions:
Achieve faster adjudication rates and reduce your
back-office workload with our automated claims
solutions.
Identify any and all missing encounters with enhanced
tracking, management and reporting for Medicare,
Medicaid, and other relevant parties.
Reduce manual data management, accelerate
workflows, and gain operational perspective for
everything from preprocessing data to integrating new
systems to accessing archived data, and more.