Introduction
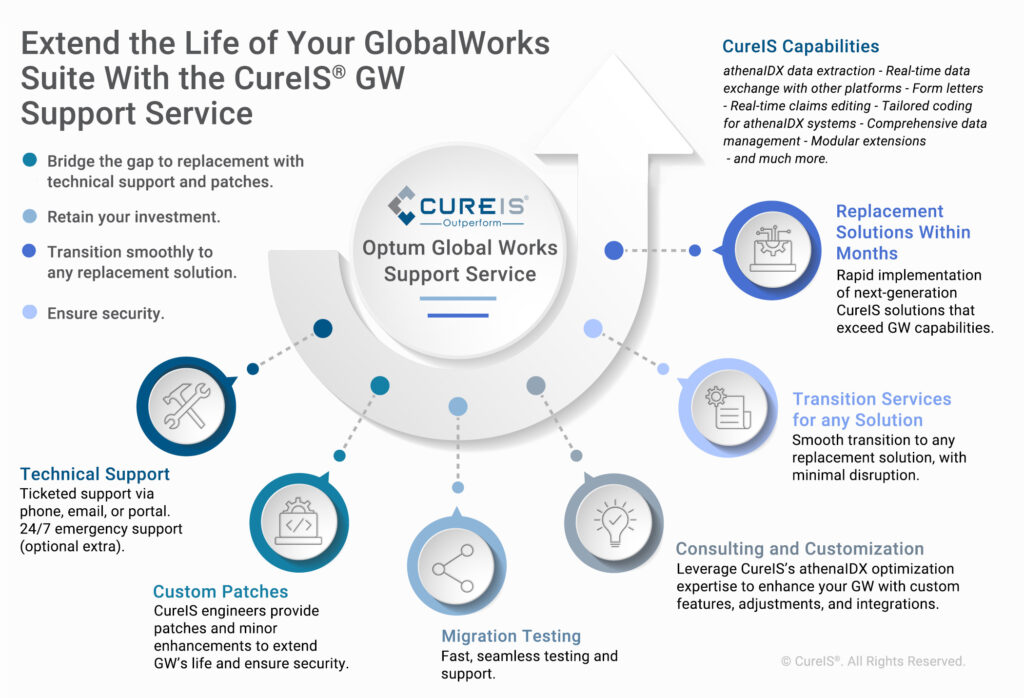
CureIS is in the business of refining healthcare operations through targeted automation and technology. Comprising a seasoned team of industry experts, CureIS leverages healthcare – focused automation and technology to process, analyze, and enhance data from any source, in any format, delivering compliance, efficiency, and effectiveness.
Background
Arizona health plans are mandated to deliver encounter data to the Arizona Health Care Cost Containment System (AHCCCS), which oversees the state Medicaid program. The delivery of accurate, compliant, and timely encounter data is crucial to satisfy regulatory requirements and to ensure the disbursement of healthcare funds is equitable, based on the real health and cost circumstances of Medicaid recipients.
Encounter data chronicles a patient’s interactions with the healthcare system. It consolidates essential details from medical claims, including patient and provider information, diagnosis codes, procedures performed, and associated cost elements.
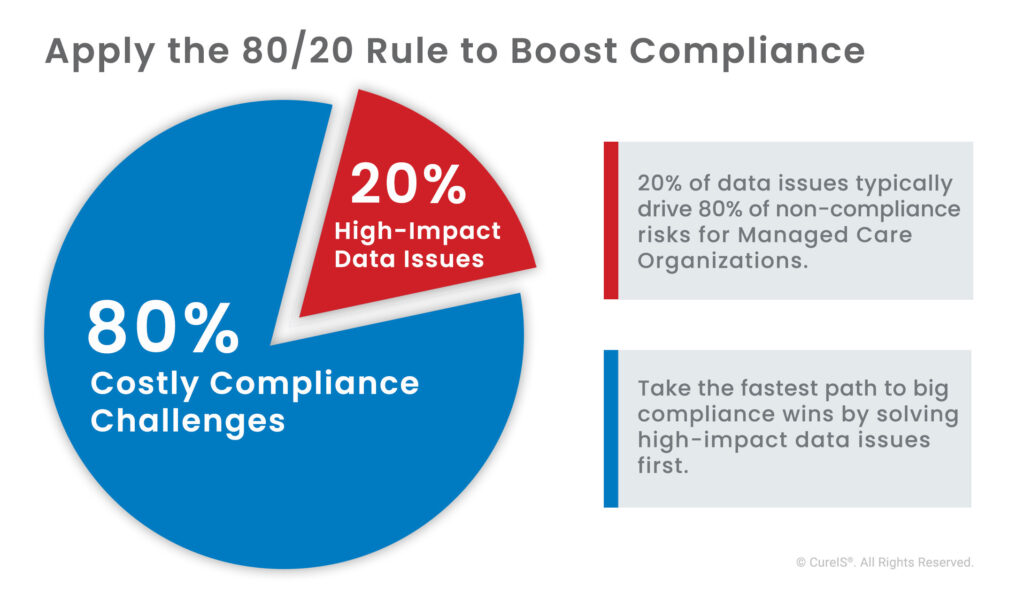
For regulatory agencies to accept this data, it must satisfy a complex set of rules that scrutinize various facets, such as the healthcare provider(s) registration status, the applicability of the services under the benefit plan, the correct handling of cost of benefits subsidies, and cost shares, as well as the proper adjudication and pricing of the claim. A health plan’s ability to receive compensation for the health services provided hinges on accurate, compliant, and timely encounter data.
Identified Challenge
A prominent Arizona health plan partnered with CureIS to address an overly manual process, citing concerns about unsustainable levels of time and money they were exerting to meet the stringent compliance standards set forth by AHCCCS and other Medicare plans.
They set their sights on two primary challenges:
- Lack of visibility into their state-mandated government programs data
- The need for a streamlined process to reduce high-cost government sanctions.
Solution
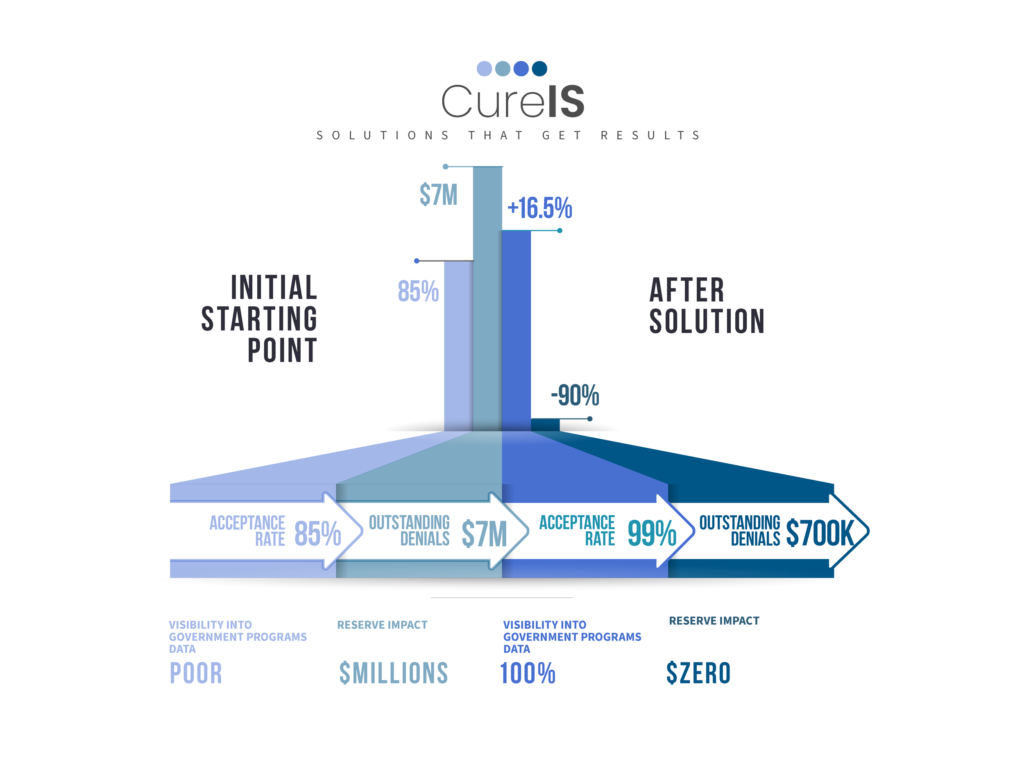
The leadership team embraced a proactive and transformative approach, collaborating with CureIS to overhaul their encounter data management system. Using EncounterCURE and ClaimsCURE on a proprietary CureIS Server, they attained 100% visibility into their encounter data and successfully reduced government-imposed sanctions from millions to $0. These results were achieved in the first 12 months.

Results
With 100% visibility into their government programs data, zero dollars in government sanctions, and a significant reduction of encounter-related financial reserves, this client has achieved impressive new levels of operational efficiency, increased compliance rates, and substantial financial savings.
“Two years ago, at this time (clean up push) we were around an 85% acceptance rate, today we are close to 99% acceptance rate. Two years ago, we had $7M in outstanding denials, today we have a little over $700k in denials. Our progress is amazing and something to be proud of.”
— Client Quote
Conclusion
CureIS empowers healthcare executives to navigate financial prudence and regulatory adherence with full visibility into your data, maximizing compliance and minimizing reserves. Unique among healthcare managed services providers,