Solutions Suite
CureIS is more than an IT company, we are problem-solvers who take accountability to the next level in our mission to deliver clean, quality healthcare data. Our team brings vast expertise to the table, from healthcare technology, operations, consulting, software, and leadership. We live our mission and values, and routinely win the “Best Places to Work” honor.
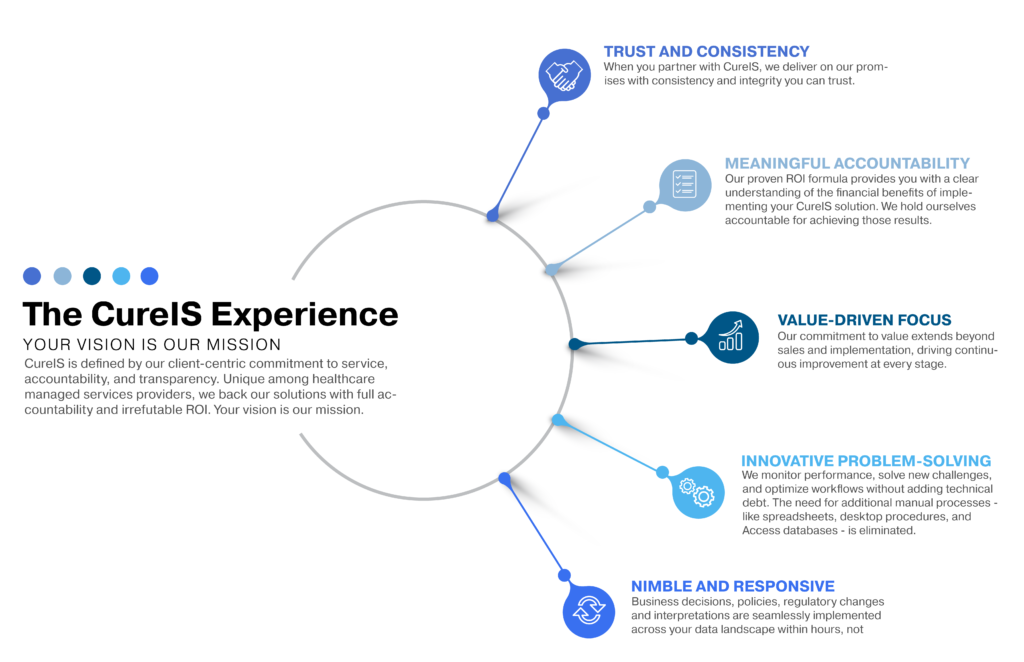
CureIS is defined by our client-centric commitment to service, accountability, and transparency. Unique among healthcare managed services providers, we back our solutions with full accountability and irrefutable ROI.
Your vision is our mission.
From enrollment to claims adjudication, payments, reconciliation, reimbursement, and compliance, CureIS provides highly specialized solutions proven to deliver savings and efficiencies most healthcare organizations never thought possible.
Learn more about the CureIS Solutions Suite.