EncounterCure
For government programs managed care,
financial success depends on encounters.
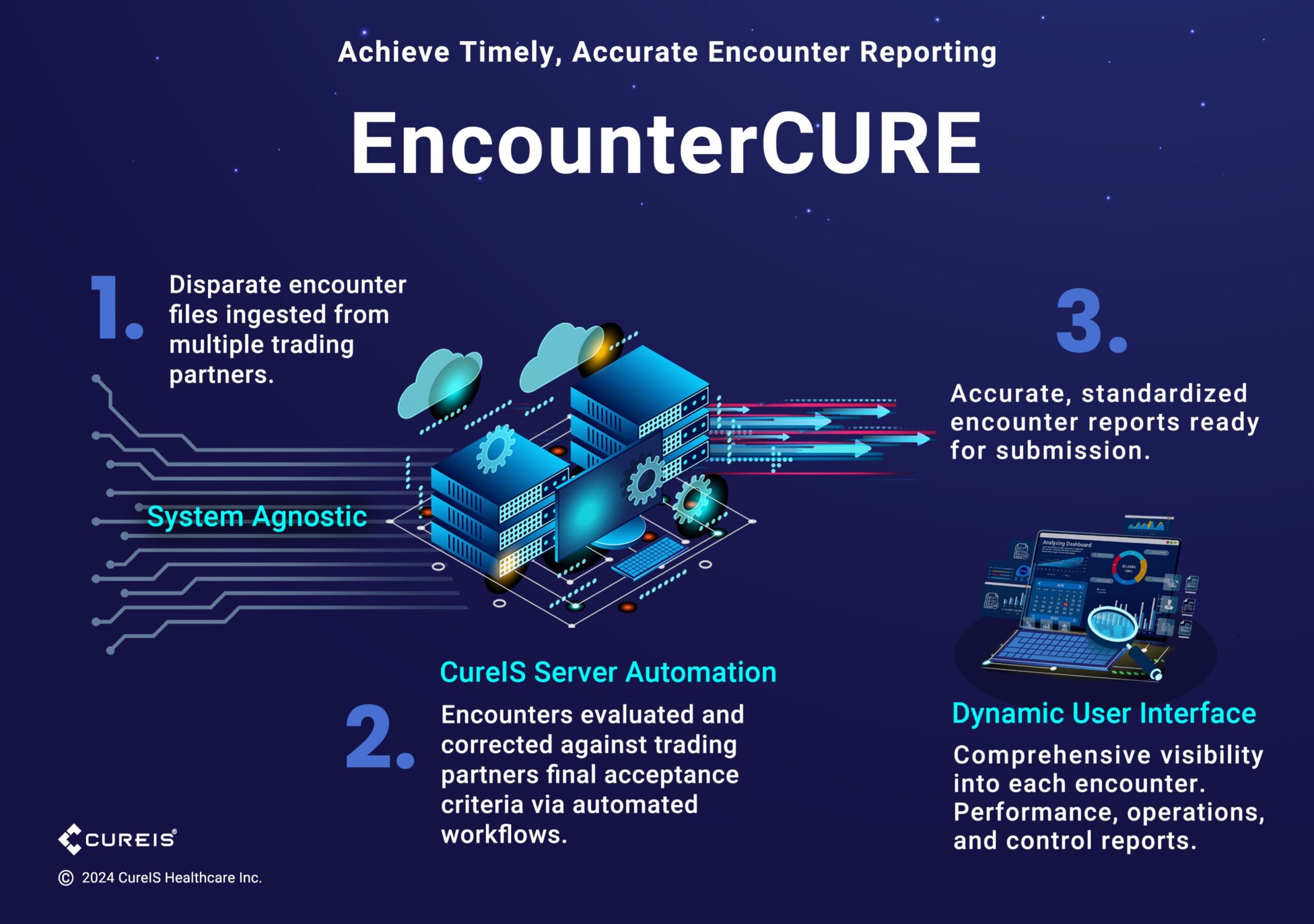
EncounterCURE ensures accuracy so you never miss an encounter.
Traditional encounter programs often come with a hefty price tag that doesn’t match the value they deliver. Most do not manage encounter responses effectively, struggle to adapt to changing rules and regulations, and only provide an incomplete picture of an organization’s financial health. If your system does not reconcile encounters against claims, you’re leaving money on the table.
EncounterCURE streamlines daily operations by promoting daily activity files that provide timely member data
- Pre-scrubs encounter submissions.
- Corrects inaccurate/incomplete data.
- Enables standardized reporting.
- Automates complex workflows.
- Rapidly assimilates regulatory changes and variable stakeholder criteria.
- Streamlines reconciliation.
Swift Implementation
The CureIS team brings years of expertise to encounter processes. Proven workflows and an extensive menu of business rules and edits enable fast implementation. Changes can be implemented and tested within hours, instead of weeks or months.
Cost Effective Efficiency
EncounterCURE integrates with unlimited data sources and enables the elimination of most manual processes. Controllable environmental challenges are addressed, lowering operating costs by reducing downstream issues that result in reprocessing, appeals, or encounter denials.
CureIS is fully accountable for ensuring results.
Explore more solutions:
Reduce your back-office workload with our automated claims
solutions.
Streamline enrollment processes and determine
eligibility accurately, consistently, and quickly.
Reduce manual data management, accelerate
workflows, and gain operational perspective for
everything from preprocessing data to integrating new
systems to accessing archived data, and more.